Health
Side Effects of this Drug are off the Charts
If it works it works. But these side effects are off the charts.
Otezla (apremilast) is a phosphodiesterase 4 (PDE4) inhibitor used to treat adult patients with active psoriatic arthritis. Common side effects of Otezla include:
diarrhea,
headache,
nausea,
upper respiratory tract infection,
vomiting,
runny or stuffy nose,
abdominal pain,
fatigue,
indigestion/heartburn,
decreased appetite,
insomnia,
back pain,
frequent bowel movements,
depression,
bronchitis,
tooth abscess, and
sinus headache.
Other side effects of Otezla include hypersensitivity, weight loss, gastroesophageal reflux disease (GERD), migraine, cough, and rash.
The recommended maintenance dosage is 30 mg twice daily taken orally starting on Day 6, after 5 days of an initial schedule of titration dosing. Otezla may interact with CYP450 inducers (such as rifampin). Tell your doctor all medications and supplements you use. During pregnancy, Otezla should be used only if prescribed. It is unknown if this drug passes into breast milk. Consult your doctor before breastfeeding.
If a person takes Otezla they may end up at the clinic below:

No vaccine? No cafe, according to new French virus law
PARIS (AP) — France’s parliament approved a law Sunday that will exclude unvaccinated people from all restaurants, sports arenas and other venues, the central measure of government efforts to protect hospitals amid record numbers of infections driven by the highly contagious omicron variant.
The National Assembly adopted the law by a vote of 215-58. Centrist President Emmanuel Macron had hoped to push the bill through faster, but it was slightly delayed by resistance from lawmakers both on the right and left and hundreds of proposed amendments.
More than 91% of French adults are already fully vaccinated, and some critics have questioned whether the “vaccine pass” will make much of a difference.
Macron’s government is hoping the new pass will be enough to limit the number of patients filling up strained hospitals nationwide without resorting to a new lockdown. New confinement measures would strike another blow to the economy — and could also cloud Macron’s chances of reelection in the April 10 presidential vote.

What is this major malfunction with anti-vaxxers? Let Darwinism handle the situation.

Dr. Ho Will Fix You Up Real Good
Dr. Ho must spend millions of dollars on advertising. He is all over television constantly on a 24 hour basis. This happy go lucky doc peddles his anti-pain remedies day and night. They must work because the ads are unrelenting therefore meaning people are buying the “cures.”

Dr. Michael Ho is a caring Doctor of Chiropractic and Acupuncture with special interest in treating patients with painful conditions relating to their muscles, joints, and nerves. He is also an engineer enthusiast who pays close attention to exercise physiology, human body mechanics, and the ill effects that bad ergonomics have on muscle, nerve, and joint-related pain. Based on his education, clinical experiences in treating his patients over the years, and in learning what his patients’ needs are, he has developed a line of self-care products that are effective for relieving pain and in helping to restore one’s health.

Covid 19: Top Ten Conspiracy Theories
Blaming 5G
This conspiracy theory should be easy to debunk: it is biologically impossible for viruses to spread using the electromagnetic spectrum. The latter are waves/photons, while the former are biological particles composed of proteins and nucleic acids. But that isn’t really the point — conspiracy theories are enticing because they often link two things which at first might appear be correlated; in this case, the rapid rollout of 5G networks was taking place at the same time the pandemic hit. Cue a viral meme linking the two, avidly promoted by anti-vaccine activists who have long been spreading fears about electromagnetic radiation, egged on by the Kremlin.
It’s worth repeating, as the World Health Organization (WHO) points out, that viruses cannot travel on mobile networks, and that COVID-19 is spreading rapidly in many countries that do not have 5G networks. Even so, this conspiracy theory — after being spread by celebrities with big social media followings — has led to cell phone towers being set on fire in the UK and elsewhere.
Bill Gates as scapegoat
Most conspiracy theories, like the viruses they resemble, constantly mutate and have several variants circulating at any one time. Many of these plots and subplots seem to involve Bill Gates, who became a new target of disinformation after gently criticizing the defunding of the World Health Organization. According to the New York Times, anti-vaxxers, members of QAnon and right-wing pundits have seized on a video of a 2015 Ted talk given by Gates — where he discussed the Ebola outbreak and warned of a new pandemic — to bolster their claims he had foreknowledge of the COVID pandemic or even purposely caused it.
A recent variant of this conspiracy theory, particularly beloved by anti-vaccination activists, is the idea that COVID is part of a dastardly Gates-led plot to vaccinate the world’s population. There is some truth in this, of course: vaccinating much of the world’s population may well be the only way to avoid an eventual death toll in the tens of millions. But anti-vaxxers don’t believe vaccines work. Instead some have spread the myth that Gates wants to use a vaccination program to implant digital microchips that will somehow track and control people. The spread of misinformation has meant that ID2020, a small non-profit that focuses on establishing digital IDs for poorer people around the world, has had to call in the FBI. (The Cornell Alliance for Science is partly funded by the Bill & Melinda Gates Foundation.)

The virus escaped from a Chinese lab
This one at least has the benefit of being plausible. It is true that the original epicenter of the epidemic, the Chinese city of Wuhan, also hosts a virology institute where researchers have been studying bat coronaviruses for a long time. One of these researchers, Shi Zhengli, a prominent virologist who spent years collecting bat dung samples in caves and was a lead expert on the earlier SARS outbreak, was sufficiently concerned about the prospect that she spent days frantically checking lab records to see if anything had gone wrong. She admits breathing a “sigh of relief” when genetic sequencing showed that the new SARS-CoV-2 coronavirus did not match any of the viruses sampled and studied in the Wuhan Institute of Virology by her team.
However, the sheer coincidence of China’s lead institute studying bat coronaviruses being in the same city as the origin of the COVID outbreak has proven too juicy for conspiracists to resist. The idea was seeded originally via a slick hour-long documentary produced by the Epoch Times, an English-language news outlet based in the United States with links to the Falun Gong religious cult that has long been persecuted by the Chinese Communist Party (CCP). The Epoch Times insists on calling COVID “the CCP virus” in all its coverage. The theory has now tipped into the mainstream, being reported in the Washington Post, the Times (UK) and many other outlets.
COVID was created as a biological weapon
A spicier variant is that COVID not only escaped from a lab, but it was intentionally created by Chinese scientists as a biowarfare weapon. According to Pew Research, “nearly three-in-10 Americans believe that COVID-19 was made in a lab,” either intentionally or accidentally (the former is more popular: specifically, 23 percent believe it was developed intentionally, with only 6 percent believing it was an accident).
This theory that the Chinese somehow created the virus is particularly popular on the US political right. It gained mainstream coverage thanks to US Sen. Tom Cotton (Republican, Arkansas) who amplified theories first aired in the Washington Examiner (a highly conservative media outlet) that the Wuhan Institute of Virology “is linked to Beijing’s covert bio-weapons program.”
This theory can be easily debunked now that there is unambiguous scientific evidence — thanks to genetic sequencing — that the SARS-CoV-2 virus has entirely natural origins as a zoonotic virus originating in bats. The Examiner has since added a correction at the top of the original piece admitting the story is probably false.
The US military imported COVID into China
The Chinese government responded to the anti-China theories with a conspiracy theory of its own that seeks to turn blame back around onto the United States. This idea was spread initially by Chinese foreign ministry spokesman Zhao Lijian, who Tweeted “it’s possible that the US military brought the virus to Wuhan.” These comments, according to Voice of America news, “echoed a rumored conspiracy, widely circulated in China, that US military personnel had brought the virus to China during their participation in the 2019 Military World Games in Wuhan last October.” For China, as the Atlantic reported, this conspiracy theory, and an accompanying attempt to rename COVID the “USA virus,”’ was a transparent “geopolitical ploy” — useful for domestic propaganda but not widely believed internationally.

GMOs are somehow to blame
Genetically modified crops have been a target of conspiracy theorists for years, so it was hardly a surprise to see GMOs blamed in the early stages of the COVID pandemic. In early March, Italian attorney Francesco Billota penned a bizarre article for Il Manifesto, falsely claiming that GM crops cause genetic pollution that allows viruses to proliferate due to the resulting environmental “imbalance.” Anti-GMO activists have also tried to blame modern agriculture, which is strange, since the known path of the virus into the human population — as with Ebola, HIV and many others — was through the very ancient practice of people capturing and killing wildlife.
Ironically, GMOs will almost certainly be part of any vaccine solution. If any of the ongoing 70 vaccine projects work (which is a big if), that would be pretty much the only guaranteed way the world can get out of the COVID mess. Vaccines could be based on either GM attenuated viruses or use antigens produced in GM insect cell lines or plants. If GMOs do help save the world from the curse of COVID, maybe they’ll stop being a dirty word.
COVID-19 doesn’t actually exist
According to professional conspiracy theorists like David Icke and InfoWars’ Alex Jones, COVID-19 doesn’t actually exist, but is a plot by the globalist elite to take away our freedoms. Early weaker versions of this theory were prevalent on the political right in the notion that the novel coronavirus would be “no worse than flu” and later versions are now influencing anti-lockdown protests across several states in the US. Because believers increasingly refuse to observe social distancing measures, they could directly help to spread the epidemic further in their localities and increase the resulting death rate.
The pandemic is being manipulated by the ‘deep state’
Some believe that a “deep state” of America’s elite is plotting to undermine the president — and that Dr. Anthony Fauci, the face of the US coronavirus pandemic response — is a secret member. Fauci’s expression of disbelief when the deep state was mentioned during a press briefing supposedly gave the game away.
COVID is a plot by Big Pharma
Many conspiracy theory promoters are in reality clever actors trying to sell quack products. Alex Jones, between rants about hoaxes and the New World Order, urges viewers to buy expensive miracle pills that he claims can cure all known diseases. Dr. Mercola, a quack anti-vax and anti-GMO medic who has been banned from Google due to peddling misinformation, claims that vitamins (and numerous other products he sells) can cure or prevent COVID. NaturalNews, another conspiracist site, sells all manner of pills, potions and prepper gear. These conspiracists depend for their market on getting people to believe that evidence-based (i.e. conventional) medicine doesn’t work and is a plot by big pharmaceutical companies to make us ill. Big Pharma conspiracies are a staple of anti-vaccination narratives, so it is hardly surprising that they have transmuted into the age of the coronavirus.
COVID death rates are inflated
Another far-right meme is the idea that COVID death rates are being inflated and therefore there is no reason to observe lockdown regulations or other social distancing measures. Prominent in promoting this myth is Dr. Annie Bukacek, whose speech warning that COVID death certificates are being manipulated has been viewed more than a quarter of a million times on YouTube. Bukacek appears in a white lab coat and with a stethoscope around her neck, making her look like an authoritative medical source. Dig a little deeper, however, as Rolling Stone magazine did, and it turns out she’s actually a far-right anti-vaccination and anti-abortion activist, previously noted for bringing tiny plastic fetuses into the Montana state legislature. Her insistence that COVID death rates are inflated has, of course, no basis in fact. More likely the current death toll is a serious under-count. T0 further clarify the issue, the Centers for Disease Control has published information about excess deaths associated with COVID-19.
Many people will believe almost anything. Covid 19 conspiracy theories demonstrates this. Believers in this nonsense get their information mainly from social media. They don’t fact check the info, they just blindly believe it.
That moron Trump started a lot of this lunacy with his “fake media” diatribes. Don’t believe mainstream media (ie NY Times, Washington Post, Wall Street Journal, CNN, CBS, NBC, ABC to name a few) just believe media outlets that support your already embedded opinions, namely Fox News.
Trump and his propaganda has deeply divided the United States. The country is in ideological turmoil. Covid-19 has caused many Americans, who believe Trump’s insane assertions, to believe the conspiracy theories no matter how ridiculous and crazy.
Covid: Moscow shops and restaurants shut in partial lockdown

Shops, restaurants and schools have shut in Moscow in a partial lockdown, as Russia battles record Covid deaths and infections.
Only essential shops like supermarkets and pharmacies are allowed to open in the capital, while food outlets are only providing takeaways.
Authorities have also given workers across Russia nine days off from Saturday in a bid to curb infections.
Russia has reported a record 1,159 deaths from Covid in the past 24 hours.
The official data also reveals 40,096 new infections in 85 regions of Russia – another record. Russia’s last major lockdown was in May-June 2020.
Russia’s overall Covid death toll in the pandemic is officially more than 230,000, the highest in Europe and one of the highest in the world.
Last October however the state statistics agency Rosstat calculated the Russian Covid death toll to be above 400,000 – far higher than the government figures.
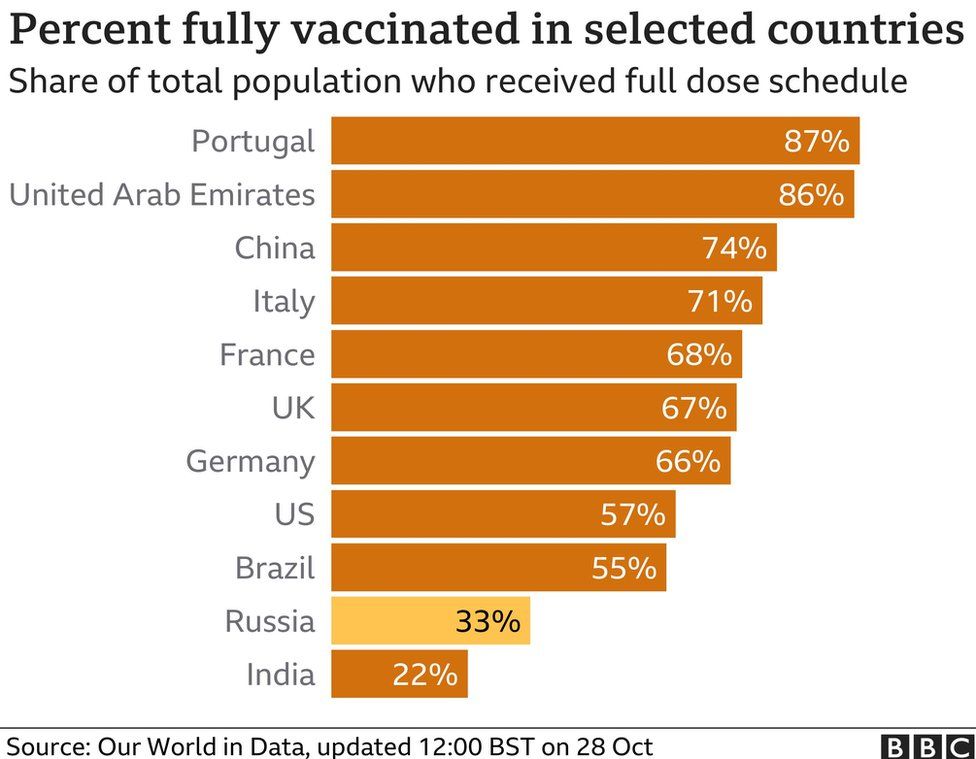
The proportion of Russia’s population fully vaccinated remains low – on 23 October it was 32.8%, Our World in Data reports. Most European countries have much higher rates.
Despite an intensive state vaccination drive, many Russians remain suspicious of the Sputnik V vaccine, which is internationally recognised as an effective shield against Covid.
Faced with this partial lockdown between 30 October and 9 November, many Russians have decided to go on holiday. Resort hotels in Egypt – a popular destination for Russians – are reported to be fully booked, and Russian flights to Egypt are sold out.
The Russian news service Vesti reports some panic-buying because of the new restrictions. There has been a rush on meat and fish at the central market in Orenburg, a city in the Urals east of Moscow.
BBC
Emotional Support Animals on Planes
An emotional support animal (ESA) is a companion animal that a medical professional has determined provides benefit for an individual with a disability. This may include improving at least one symptom of the disability. Emotional support animals, typically dogs, but sometimes cats or other animals, may be used by people with a range of physical, psychiatric, or intellectual disabilities. In order to be prescribed an emotional support animal the person seeking such an animal must have a verifiable disability. To be afforded protection under United States federal law, a person must meet the federal definition of disability and must have a note from a physician or other medical professional stating that the person has that disability and that the emotional support animal provides a benefit for the individual with the disability. An animal does not need specific training to become an emotional support animal.

The Air Carrier Access Act establishes a procedure for modifying pet policies on aircraft to permit a person with a disability to travel with a prescribed emotional support animal, so long as they have appropriate documentation and the animal is not a danger to others and does not interfere with others (through unwanted attention, barking, inappropriate toileting, etc.

CNBC
Want to travel with an emotional support dog, duck or miniature horse? Starting next month, United Airlines will want passengers to show they can behave.
The airline is setting more stringent requirements for emotional support animals, joining Delta Air Lines in cracking down on a sharp increase in such animals in the cabin. Delta complained that some of the animals soiled cabins or bit travelers.
United said the number of customers bringing emotional support animals on board has risen 75 percent over the past year.
“The Department of Transportation’s rules regarding emotional support animals are not working as they were intended to, prompting us to change our approach in order to ensure a safe and pleasant travel experience for all of our customers,” United said.
Late last month, a Brooklyn artist tried to bring a peacock on board a cross-country United flight, but was turned away by the airline because of the bird’s weight and size.

“As a reminder, animals currently prohibited from traveling in the cabin include hedgehogs, ferrets, insects, rodents, snakes, spiders, reptiles, sugar gliders, non-household birds, exotic animals and animals not properly cleaned or carry a foul odor,” said United.
The animals below are not on the prohibited list.


Last 2 images above courtesy of Markozen photoshop.
Smoking Rates by Country

76 percent of men in Indonesia smoke!
Data is for 2015.
| Country | Total Smoking Rate | Male Smoking Rate | Female Smoking Rate |
|---|---|---|---|
| Kiribati | 52.40% | 63.90% | 40.90% |
| Nauru | 47.50% | 43.00% | 52.00% |
| Greece | 42.65% | 52.60% | 32.70% |
| Serbia | 41.65% | 43.60% | 39.70% |
| Russia | 40.90% | 59.00% | 22.80% |
| Jordan | 40.45% | 70.20% | 10.70% |
| Indonesia | 39.90% | 76.20% | 3.60% |
| Bosnia And Herzegovina | 38.60% | 47.20% | 30.00% |
| Lebanon | 38.20% | 45.40% | 31.00% |
| Chile | 38.00% | 40.00% | 36.00% |
| Latvia | 36.60% | 48.90% | 24.30% |
| Croatia | 36.45% | 39.40% | 33.50% |
| Sierra Leone | 36.00% | 60.00% | 12.00% |
| Bulgaria | 35.30% | 42.40% | 28.20% |
| Cuba | 35.25% | 52.70% | 17.80% |
| Austria | 35.15% | 35.50% | 34.80% |
| Czech Republic | 33.20% | 37.40% | 29.00% |
| Estonia | 33.05% | 41.20% | 24.90% |
| Laos | 32.85% | 56.60% | 9.10% |
| Andorra | 32.50% | 37.20% | 27.80% |
| Georgia | 31.70% | 57.70% | 5.70% |
| Ukraine | 31.70% | 49.40% | 14.00% |
| Germany | 30.35% | 32.40% | 28.30% |
| Israel | 30.25% | 41.20% | 19.30% |
| Tonga | 30.15% | 47.30% | 13.00% |
| Lithuania | 30.15% | 38.10% | 22.20% |
| Samoa | 29.95% | 41.00% | 18.90% |
| Romania | 29.80% | 36.90% | 22.70% |
| Albania | 29.40% | 51.20% | 7.60% |
| Spain | 29.20% | 31.30% | 27.10% |
| Slovakia | 28.65% | 39.70% | 17.60% |
| Belarus | 28.40% | 46.20% | 10.60% |
| Hungary | 28.40% | 32.00% | 24.80% |
| Bahrain | 28.20% | 48.80% | 7.60% |
| Poland | 28.05% | 32.40% | 23.70% |
| Lesotho | 27.75% | 55.10% | 0.40% |
| France | 27.70% | 29.80% | 25.60% |
| Kyrgyzstan | 27.00% | 50.40% | 3.60% |
| South Korea | 27.00% | 49.80% | 4.20% |
| Armenia | 26.90% | 52.30% | 1.50% |
| Kazakhstan | 26.60% | 43.90% | 9.30% |
| Mongolia | 26.50% | 47.70% | 5.30% |
| Turkey | 25.95% | 39.50% | 12.40% |
| Seychelles | 25.90% | 43.00% | 8.80% |
| Philippines | 25.75% | 43.00% | 8.50% |
| Fiji | 25.55% | 38.70% | 12.40% |
| Moldova | 25.55% | 45.70% | 5.40% |
| Namibia | 25.15% | 38.90% | 11.40% |
| Egypt | 25.10% | 49.90% | 0.30% |
| Netherlands | 25.05% | 26.20% | 23.90% |
| Malta | 24.95% | 29.70% | 20.20% |
| China | 24.70% | 47.60% | 1.80% |
| Vietnam | 24.20% | 47.10% | 1.30% |
| Nepal | 24.10% | 37.10% | 11.10% |
| Italy | 24.00% | 28.30% | 19.70% |
| Argentina | 23.95% | 29.50% | 18.40% |
| Mauritania | 23.85% | 44.00% | 3.70% |
| Bolivia | 23.80% | 30.50% | 17.10% |
| Luxembourg | 23.60% | 25.80% | 21.40% |
| Azerbaijan | 23.45% | 46.50% | 0.40% |
| Cambodia | 23.45% | 44.10% | 2.80% |
| Morocco | 23.40% | 45.40% | 1.40% |
| Switzerland | 23.30% | 26.90% | 19.70% |
| Belgium | 23.25% | 26.50% | 20.00% |
| Uruguay | 23.05% | 26.70% | 19.40% |
| Portugal | 22.60% | 31.50% | 13.70% |
| Republic Of The Congo | 22.45% | 43.20% | 1.70% |
| Pakistan | 22.45% | 41.90% | 3.00% |
| Cameroon | 22.35% | 43.80% | 0.90% |
| Norway | 22.25% | 22.40% | 22.10% |
| Malaysia | 22.20% | 43.00% | 1.40% |
| Japan | 22.15% | 33.70% | 10.60% |
| Ireland | 22.15% | 22.40% | 21.90% |
| Thailand | 21.85% | 41.40% | 2.30% |
| Mauritius | 21.70% | 40.10% | 3.30% |
| Finland | 20.85% | 23.20% | 18.50% |
| Sweden | 20.60% | 20.40% | 20.80% |
| Burkina Faso | 20.25% | 36.00% | 4.50% |
| Bangladesh | 20.25% | 39.80% | 0.70% |
| Slovenia | 20.20% | 22.30% | 18.10% |
| Mali | 20.00% | 36.80% | 3.20% |
| United Kingdom | 19.15% | 19.90% | 18.40% |
| Myanmar | 19.00% | 31.60% | 6.40% |
| South Africa | 18.95% | 31.40% | 6.50% |
| Mozambique | 18.65% | 31.40% | 5.90% |
| Paraguay | 18.10% | 28.30% | 7.90% |
| Jamaica | 17.90% | 29.90% | 5.90% |
| Honduras | 17.70% | 33.30% | 2.10% |
| United States | 17.25% | 19.50% | 15.00% |
| Denmark | 17.00% | 17.60% | 16.40% |
| Zimbabwe | 16.65% | 31.20% | 2.10% |
| Singapore | 16.50% | 28.00% | 5.00% |
| Brunei | 16.20% | 29.30% | 3.10% |
| Iceland | 16.05% | 17.00% | 15.10% |
| Niue | 15.85% | 20.30% | 11.40% |
| Malawi | 15.70% | 25.40% | 6.00% |
| Tanzania | 15.65% | 27.50% | 3.80% |
| Zambia | 15.55% | 26.50% | 4.60% |
| Saudi Arabia | 15.40% | 27.90% | 2.90% |
| Brazil | 15.30% | 19.30% | 11.30% |
| Liberia | 15.00% | 27.60% | 2.40% |
| Canada | 14.95% | 17.70% | 12.20% |
| Australia | 14.90% | 16.70% | 13.10% |
| Comoros | 14.55% | 23.10% | 6.00% |
| Sri Lanka | 14.40% | 28.40% | 0.40% |
| Dominican Republic | 14.10% | 18.80% | 9.40% |
| Mexico | 13.70% | 20.80% | 6.60% |
| Costa Rica | 13.40% | 18.50% | 8.30% |
| Kenya | 13.35% | 24.60% | 2.10% |
| Uzbekistan | 13.10% | 24.90% | 1.30% |
| Cape Verde | 12.85% | 22.20% | 3.50% |
| Haiti | 12.30% | 22.10% | 2.50% |
| Senegal | 12.05% | 23.40% | 0.70% |
| India | 11.15% | 20.40% | 1.90% |
| Colombia | 11.10% | 16.00% | 6.20% |
| Iran | 11.10% | 21.50% | 0.70% |
| Oman | 11.00% | 21.00% | 1.00% |
| Eswatini | 10.60% | 19.00% | 2.20% |
| Uganda | 9.65% | 16.40% | 2.90% |
| Niger | 9.40% | 18.60% | 0.20% |
| Benin | 9.35% | 17.70% | 1.00% |
| Nigeria | 9.25% | 17.40% | 1.10% |
| Ecuador | 8.65% | 14.00% | 3.30% |
| Barbados | 7.00% | 13.10% | 0.90% |
| Ghana | 6.75% | 13.10% | 0.40% |
| Panama | 6.60% | 10.60% | 2.60% |
| Ethiopia | 4.70% | 8.90% | 0.50% |
Source: World Population Review 2021
